Leishmaniasis is the type of disease you really don’t want to get.
Caused by a parasite spread by sandflies, cases first appear as bumps or lumps which may end up as ulcers, which no less than the U.S. Centers for Disease Control and Prevention described as “a volcano.” One form of the disease can wreak havoc on internal organs like the liver, spleen, and bone marrow—and can do so with symptoms that may not develop until years after the long-forgotten bite.
Various genetic tests can detect and identify the parasite and species type, and blood tests can detect an antibody. Skin sores may heal on their own, but healing may take months, and ugly scars can be left behind. Advanced untreated cases of visceral leishmaniasis are usually fatal. There’s no vaccine or drug to prevent infection—if you want to avoid leishmaniasis, the best advice is to avoid outdoor activities, especially between dusk and dawn, to apply insect repellent, and to minimize the amount of exposed skin by wearing long-sleeve shirts, long pants, and socks. So much for that beach tan.
Leishmaniasis has been recorded through the ages, with descriptions of the sore found in tablets in the 7th century library of the Assyrian King Ashurbanipal. It was mentioned in ancient Egyptian documents and chronicled by Persian scientists before 1000 AD. More recently, epidemics were reported during the Syrian civil war and refugee crisis.
Early cultures experimented with a type of inoculation for the disease. As explained in one report, “They inoculated exudates from active lesions into the buttocks of young children, particularly girls, or exposed the bottoms of babies to sand flies to prevent the development of disfiguring facial scars.” But the practice occasionally resulted in skin lesions and is no longer practiced, and any better solution has evaded researchers—until now.
Forget primitive inoculations. Gene editing may provide a solution.
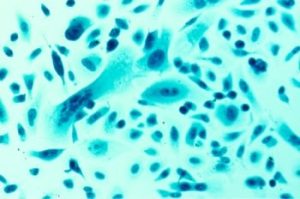
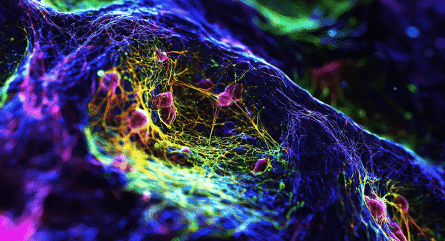
In 2020, an international team of researchers engineered the Leishmania parasite's genome using CRISPR-Cas technology to limit its infectivity and allow it to be given as a vaccine, creating long-term immunity without causing the disease. The CRISPR experiment was performed in mice.
The result is a “second generation leishmanization live vaccination with an attenuated L. major strain (LmCen−/−) that does not cause lesions but retains the ability to provide immunological protection against experimental needle and sand fly transmitted Leishmania infection. As LmCen−/− is marker-gene-free safe and efficacious, it can be advanced to Phase I human clinical trials.”
It’s important to note that this new, edited version does not have antibiotic resistance—a critical feature required by regulatory agencies.
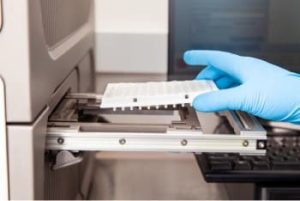
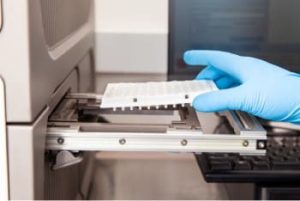
CRISPR-Cas was essential to creating the marker-free strain, the researchers wrote, as it could delete genes with high specificity and fidelity. Analysis by whole genome sequencing confirmed the precise deletion but no detectable off-target mutations.
CRISPR improves the design of experimental vaccine approaches
The application of CRISPR genome editing to this common plague—leishmaniasis affects some 2 million people each year—is just one way that the emerging technology is being applied to vaccine development.
“The application of CRISPR/Cas9 provides a novel platform in the development of recombinant viral vaccines through improvements in vaccine design and experimental vaccination approaches across different species,” noted a review in Frontiers in Cellular and Infection Microbiology. “CRISPR/Cas9 provides an alternative method to conventional approaches which is fast, efficient, and straightforward.”
“Researchers are using CRISPR-Cas9 to genetically reprogram B cells to produce—and keep producing—the needed antibody, explained an article in Stat.
Despite decades of effort, the Stat article added, there have been no vaccines to fight common, deadly afflictions like HIV, the Epstein-Barr virus, and respiratory syncytial virus. The reasons why include the difficulty identifying the exact piece of antigen that will trigger the production of an effective antibody and the failure of existing vaccines when B cells don’t arrange their DNA segments in the precise way to manufacture the necessary antibodies. Antibodies, for example, can control the viral loads in people with HIV but only last for a few weeks. The solution? Use CRISPR-Cas9 to genetically reprogram B cells to produce and keep producing whatever antibody it is that is needed.
HIV is emerging as a major application area for CRISPR vaccine development. In a study published early in 2020, researchers noted the rapid progress of CRISPR-Cas9 HIV-1 therapy research in recent years.
“The first CRISPR/Cas9 application in the prevention of HIV-1 infection was performed in 2013 by disruption of latent HIV-1 provirus,” they wrote. “From then on, numerous studies on HIV-1/AIDS gene therapy by CRISPR/Cas9 technology have been reported, suggesting its tremendous potential to treat HIV-1/AIDS.”
They noted that CRISPR technology offers more convenient and efficient target site design, easier vector construction, limited CRISPR off-target effects, and quick applications in research settings.
CRISPR eyed for combat against malaria and avian viruses
CRISPR is also emerging as a promising tool for the development of a malaria vaccine.
CRISPR has been shown to be a more cost-effective and possibly quicker and more efficient way to battle malaria, with CRISPR applied to the parasite’s life cycle to spread antimalarial genes into a vector population.
“By revolutions in functional genomics and related approaches, the role of different genes in pathogenesis have been determined and these data pave the road for creation of specific mutant parasites,” noted one study in Vaccines & Vaccination. “The arms of this strategy are the genetic engineering methods. CRISPR/Cas9 is a promising and new method which has been introduced as an efficient tool for targeted gene manipulation in different organisms.”
CRISPR is also being put to work to understand avian viruses and develop vaccines for poultry. Not only are chickens useful models for different fields of research, but such a vaccine could help secure an important global food source.
CRISPR offers a simpler, faster, and effective alternative for developing viral vector vaccines in animals, noted Frontiers in Cellular and Infection Microbiology. So far, it’s been put to use in the targeted mutagenesis of viral vectors, including turkey herpesvirus, infectious laryngotracheitis virus, and duck enteritis virus. Other efforts are targeting the Newcastle disease virus, avian influenza virus, and Marek’s disease virus.
After success in animals, studies change aim to humans
While most CRISPR models have been in animals, the application of the technology is slowly advancing—with success. Already, CRISPR technology has been used to target a rare inherited disease that causes blindness and to treat a patient with sickle cell disease. More recently, researchers have turned to CRISPR to possibly develop a vaccine for multiple sclerosis.
The idea of such a vaccine took root as early as 2008, when it was recognized that a number of cell types played a role in the disease’s initiation and perpetuation.
More—perhaps much more—is in the works. In November 2020, Eli Lilly and Company announced a plan to use Precision Biosciences’ ARCUS genome editing platform to research and develop potential in vivo therapies for genetic disorders such as Duchenne muscular dystrophy. CRISPR Therapeutics and Vertex Pharmaceuticals are reportedly continuing work on their clinical studies of gene editing to tackle sickle cell disease. And in April of 2020, a Nature study reported the identification of genes that could be clinically manipulated so that, in autoimmune diseases, a body’s immune system would not attack itself.
And what of the future of the leishmaniasis vaccine? One of the study’s authors told New Atlas that the vaccine, when it is available, could cost less than $5 a dose, which would bring hope to some of the impoverished tropical countries where the disease is most prevalent.