Is genetic testing a culprit in unnecessary ovary removal procedures?
In May, researchers from the University of Pennsylvania, led by Susan Domchek, announced findings from a study showing that women with gene variants not known to increase the risk of ovarian cancer, and with no personal or family history of the disease, still had surgery to remove their ovaries in an attempt to reduce their cancer risk. The findings, wrote 360dx, suggest “that patients and their doctors do not fully understand the genetic test results.”
Genetic testing can help patients and their doctors learn about inherited or acquired gene variants linked to cancer. When offered in connection with genetic counseling, results can inform preventative care, such as lifestyle changes like diet, exercise, or smoking cessation, to reduce an individual’s risk factors for cancer. When genetic testing confirms inherited risk factors and a patient and her family’s health histories offer further proof of an elevated risk for disease, preventive medical measures are sometimes considered.
One preventive medical procedure is ovary removal, typically performed through open surgery or laparoscopic or robot-assisted operations. Risks include bleeding and infection, along with a reduced or eliminated ability to become pregnant. Between 2005 and 2014, ovary removal surgery, called oophorectomy, fell from about 123.1 visits per 100,000 adult women to 108.4 per 100,000; the reason for the decline was not clear.
Next generation sequencing tests required nuanced assessments
Data suggesting that some ovary removal procedures were unnecessary were drawn from the Prospective Registry of Multiplex Testing.
“Out of the 4,589 women who received oophorectomy … Domchek and colleagues identified 457 patients, or 10%, who did not fall under expert guidelines for preventive surgery based on their ovarian cancer risk,” noted 360dx. “Specifically, 114, or 16 percent, of 731 women with a VUS [variant of uncertain significance] in a high-risk ovarian cancer gene reported oophorectomies. Expert guidelines recommend against making clinical decisions based on VUS.
"These data raise the concern that there are some women who are undergoing preventive oophorectomy, who are often under age 50 [and potentially premenopausal] without clear indications," Domchek said during a presentation, adding that if these findings are validated, then it suggests the potential for harm.
While some of the data from the study were self-reported, 360dx notes that as large next generation sequencing (NGS) panels become more popular as a gauge for assessing cancer risk in the broader population, physicians must “navigate complex, evidence-based guidelines around specific genes they're unfamiliar with. Beyond a handful of ‘famous’ genes, such as BRCA1 and BRCA2, many oncologists may not know the nuances of the cancer risk data associated with the dozens or hundreds of other genes now included in NGS panels.”
Molecular information yields new treatment options
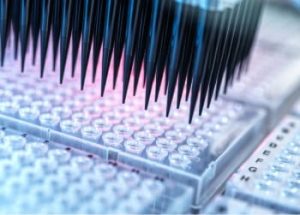
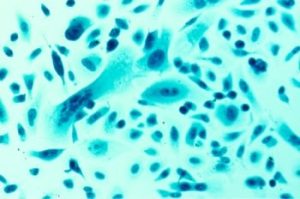
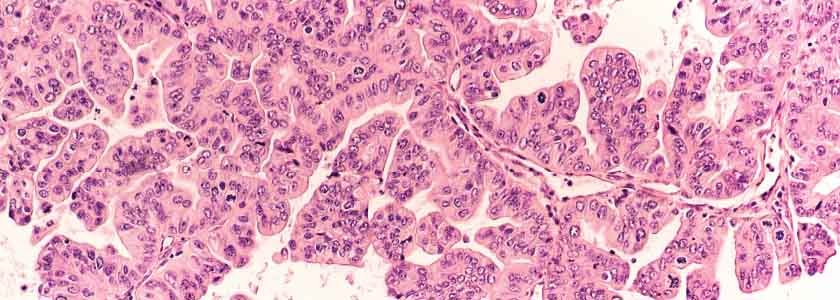
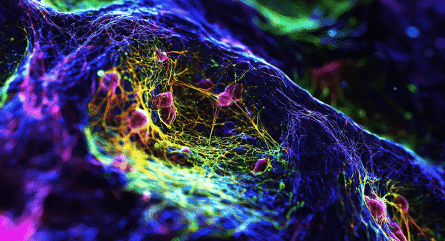
In addition to assessing the risk for ovarian cancer, molecular information is also helping to identify new treatment strategies. In June, a team, led by Broad Institute researchers, found inhibiting the JAK/STAT pathway in laboratory models to be a potential treatment strategy for high-grade serous ovarian cancer (HGSOC) using single-cell RNA sequencing. The Janus kinase (JAK)-signal transducer and activator of transcription (STAT) pathway “plays critical roles in the orchestrating of immune systems, especially cytokine receptors, and they can modulate the polarization of T helper cells,” explains an article in Cell Communication and Signaling.
The Broad Institute’s Aviv Regev used single-cell RNA sequencing to analyze about 11,000 cells from ascites of ovarian cancer patients. “About a third of ovarian cancer patients have ascites—a build up of abdominal fluid—at diagnosis, and it is associated with drug resistance and a poor prognosis,” explained Genome Web. “Recurrent ovarian cancer is associated with a median survival of about a year. While the researchers uncovered inter-patient variability in the makeup and function of the cells in the ascites samples, they also noted the shared expression of inflammatory programs.”
The study was reported in Nature Medicine. Researchers further found that an inhibitor targeting the JAK/STAT pathway, which is expressed in both malignant and cancer-associated fibroblast cells, had antitumor activity in cell cultures and patient-derived tissue grafts or organ transplants.
Through high-throughput screening for compounds active in this target, researchers identified JSI-124 for further analysis as a pathway inhibitor in ovarian cancer.
"Together, these results suggest that JAK/STAT inhibition may be a potent therapeutic option for patients with high-grade serous ovarian cancer, through action on malignant cells, non-malignant cells, or both," Regev and her colleagues wrote in their paper.
Despite challenges, NGS offers promise for personalized cancer treatment
The ability of NGS to deliver personalized cancer treatment is nothing new—a team of Chinese researchers, for example, noted in 2012 that NGS in cancer treatment offered high throughput at a low cost. A 2015 study, meanwhile, explained how new therapies that target somatically muted genes identified by clinical NGS were gaining approval from the U.S. Food and Drug Administration and that new clinical trail designs were weighing histology equally with genetic identifiers.
So when should an NGS test be ordered for a patient with cancer?
“When and how to use NGS testing in the clinic is at present an unsolved issue, although new research results provide evidence favoring this approach in some types of advanced cancer,” a 2020 study published in The Lancet stated.
To get it right, physicians need to know the clinical evidence behind new biomarkers to use NGS at the right moment.
“NGS-enabled precision oncology is adding a new layer of complexity to daily clinical decision making,” the study added. “As with any other laboratory test, doctors and patients must be sure before ordering an NGS test that its result will have an impact of the therapeutic plan. In any case, standard single-gene molecular testing must always be performed when indicated, since important therapeutic targets might be potentially missed if no molecular analyses were performed.”